Paul Richards, emeritus professor of Technological and agricultural development, has known Sierra Leone for 40 years, His wife comes from there and since retiring he has been adjunct professor at Njala University in the middle of the country. Born near Manchester in the UK, Richards visited the West African country for the first time in 1977. He researched agricultural practices there until civil war broke out in 1991. Then he turned his attention to describing the situation and went on to study the country’s recovery from the war.
This pattern more or less repeated itself in 2014. When the ebola epidemic broke out, Richards and Wageningen development economist Maarten Voors were in the midst of research on living conditions and nature conservation in Sierra Leone. Voors and the students went home but Richards stayed. ‘I knew what prophylactic measures I should take,’ he emails from Sierra Leone. He and Voors decided to study the social factors underlying the epidemic. ‘After all, this virus is spread from person to person.’
The results of this and other social-science research are published on the Ebola Response Anthropology Platform (ERAP), which Richards set up with British colleagues. This gives policymakers and medical personnel access to a supply of information which contributes to controlling the virus.

Paul Richards
Social intimacy
Ebola is a disease of ‘social intimacy’ and a ‘crisis for family-based care’, the researchers make clear. The virus is spread through direct contact with blood, faeces, urine, sperm, vomit and sweat. The main infection routes are the care of the sick and the laying out of the dead. These tasks are carried out by close family because the patients trust them. When you are in crisis you go home to your family.
People sometimes pay a high price for answering the call of duty in the context of ebola: they fall sick themselves. Yet demands for a protocol for homebased care initially fell on deaf ears, says Richards. ‘That was considered unthinkable by the authorities. The necessity of it only dawned on them later.’
Access to land or other property and obligations related to the deceased also played a role in the spread of the disease. ‘There are social and spiritual aspects to burying the dead,’ writes Richards in his book. ‘Hatchets are buried and debts written off.’ At a wedding, presents and services are pledged to the parents and family of the bride. If when she dies they have still not been delivered – which is often the case – the woman is buried with her own family. The virus is also spread through travel for education, migration, trade or medical treatment.
People’s science
Richards and his colleagues also conducted a survey from December 2015 to find out what exactly happened during the Ebola outbreak. The epidemic was at its peak at that point but the researchers visited villages in a region where the disease had already run its course. The results make clear how infections progress and how all kinds of rumours gather momentum and then blow over just as fast. ‘In response to the reality of the disease people learned to think like epidemiologists,’ concluded Richards. ‘In one of the villages the researchers visited, appropriate action by the villagers had practically wiped out the disease before international aid workers reached the village.
This is what Richards means by ‘people’s science’ in the subtitle of his recently published book on the ebola crisis. ‘It refers to every tendency a community shows to look at a problem situation in a new light on the basis of empirical evidence.’ The opposite tendency was seen in the Brexit debate and during the American presidential election campaigns, where gut feelings took precedence over hard evidence. In the battle against ebola too, gut feelings were influential at first and experts were regarded with suspicion. But my book shows that this changed when affected communities started thinking about the pattern of infection that was observable. This was ‘people’s science’ because the result depended on local knowledge about social relations which is not transparent to outsiders.’
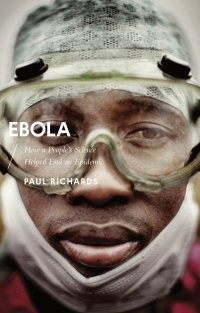
Paul Richards, Ebola. How a people’s science helped end an epidemic, Zed Books, ISBN 978-1-78360-858-4
Resistance
With an infectious disease such as ebola it is important that patients and healthcare workers agree on the important steps for preventing new cases, says Richards. ‘But all the action that needs to be taken to stem ebola, from identification and isolation to safe burial, sometimes encounters resistance. That is why is it so important to find out how care is delivered and how people are buried. From that you can deduce where there is scope to change customary practices,’ states Richards in his book. ‘If local people are the main carers, they don’t feel the need for anthropologists,’ he explains. ‘But that changed when the international community got involved. The focus shifted towards logistics, organization and control, which made it counterproductive. International aid workers wanted to ban burials, for instance, because they could be a source of infection. We explained why that would never work, and that it was better to work towards what would come to be known as a safe and dignified burial.’
The ebola anthropology platform ERAP received the Outstanding International Impact Prize from the British Economic and Social Research Council (ESRC) in June 2016. Richards was delighted. ‘This is a recognition of the importance of anthropological knowledge.’

